 Leah Hennig
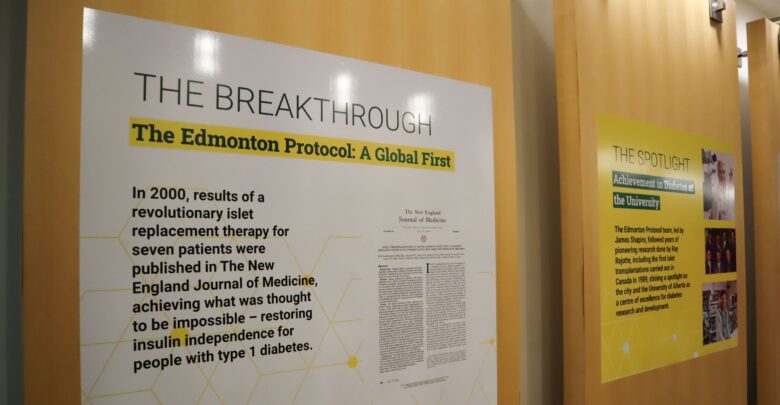
Leah HennigThe University of Alberta held an event on June 4 to celebrate the 25th anniversary of the Edmonton Protocol. The Edmonton Protocol research proved that islet transplantations could be a successful method of treating Type 1 diabetes.
Since the Edmonton Protocol was originally published in the New England Journal of Medicine in 2000, work on improving islet transplants for those with Type 1 diabetes has continued.
In Edmonton, 330 patients have received islets transplants, and more than 3,000 transplants have taken place across the world.
Bill Flanagan, president and vice-chancellor of the U of A, spoke at the event celebrating the 25th anniversary.
“This has been a groundbreaking and a life changing advancement in diabetes research that has garnered worldwide attention,” Flanagan said.
“As a research-intensive university, this is where remarkable talent advanced new frontiers of knowledge and discovery.”
He said the Edmonton Protocol is often an example he used to talk to alumni, donors, and government about the impact the U of A has.
“When we got to patient number seven, we knew we had something quite spectacular,” Dr. Shapiro says
Dr. James Shapiro was the lead author on the original paper. Shapiro was working on cell transplants as a medical student at the University of Newcastle when he became interested in islet transplants. He began working on the new protocol on March 11, 1999 at the U of A.
“We transplanted our first patient, Byron Best, and when we put enough cells into him, he was able to come off insulin,” Dr. Shapiro said in an interview with The Gateway. “The next six patients all came off insulin. And then we knew when we got to patient number seven, we had something quite spectacular.”
He wrote the paper in the New England Journal of Medicine, which was published on July 27, 2000.
“It caused quite the storm,” he said. “It actually shut the hospital switchboard down for about three or four days. Patients all around the world [were] scrambling to get on the transplant list.”
Dr. Shapiro said they’ve had a very successful program since. They are now trying to see if they can do the islet transplants without the need of anti-rejection drugs that patients who receive a transplant have to take.
He also said they’re hoping in the future, they’ll be able to do transplant trials with stem cell islets made from patient’s own bodies so there isn’t a need for the anti-rejection drugs.
“The Edmonton Protocol is proof of concept that the cell transplant could potentially, one day, cure diabetes, and that’s what all of this is about,” Dr. Shapiro said.
“I have no doubt that I’m alive today because of it,” Teskey says
According to Diabetes Canada, about 10 per cent of people with diabetes are Type 1 and are insulin-dependent. In order to control their glucose levels in their blood, they have to inject insulin regularly.
Bob Teskey was patient four out of seven in the Edmonton Protocol. He also previously worked at the U of A law firm and was a member of the Board of Governors from 2009–2016.
Teskey told The Gateway that he’d lived with diabetes for about 40 years by the time he got the transplant.
“I was really having difficulties with what we call undetected lows and so you’d just pass out,” he said.
Teskey said it took three transplants and then he was completely off insulin for four years. He takes some insulin now, but said that even after 27 years the cells are still working so he’s able to take less.
“I have no doubt that I’m alive today because of it,” Teskey said. “If I hadn’t had it, I think the various complications that come with long-term insulin [use] would have killed me.”
He also said the Edmonton Protocol really put the U of A on the map.
“It’s still something that is mentioned in the story of the university that goes out publicly,” Teskey said.