 Supplied
SuppliedA University of Alberta research team is testing a graft technology that will deliver anti-rejection immunosuppression drugs to newly transplanted islet cells. By localizing the drugs to just the islet cells, this would help make these transplantations safe and accessible to individuals living with Type 1 diabetes (T1D).
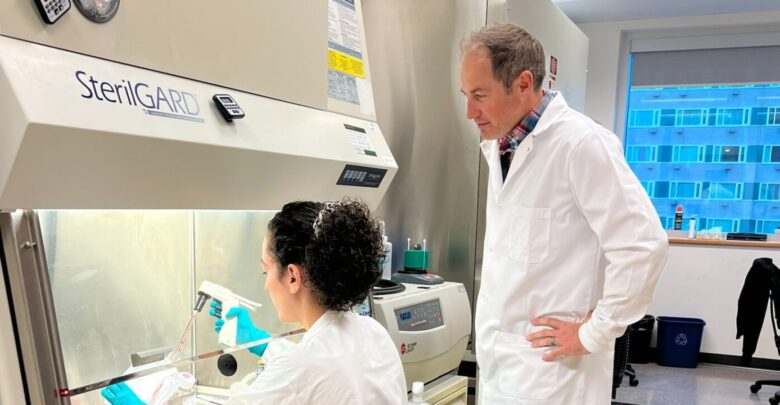
The study is being led by Andrew Pepper, an assistant professor in the department of surgery and Canada Research Chair in Cell Therapies for Diabetes. He is collaborating with Greg Korbutt, a professor in the department of surgery and scientific director of Alberta Cell Therapy Manufacturing. As well, Pepper is working with research associate Purushothaman Kuppan. The team has recently received a Canadian Institutes of Health Research grant of $1,082,476 to conduct this study. The grant will span over five years.
T1D is an auto-immune disease. It develops when the immune system mistakenly destroys the insulin-producing beta cells within islet cells in the pancreas. This leaves the pancreas incapable of producing insulin.
Insulin is a regulatory hormone necessary for glucose uptake by cells for energy production. Impaired insulin function can lead to complications affecting vital organs of the body.
For people whose diabetes can’t be treated with insulin, islet cell transplantations are the last resort, Pepper says.
T1D, which has no cure, affects an estimated 300,000 Canadians. Available treatments only focus on managing complications from the disease.
For treating T1D, Pepper said that insulin is still the main treatment, either through needle injection or an artificial pancreas.
“In individuals that unfortunately have failed on all the different [treatment options], the last line of defense is an islet transplant,” he said.
According to Pepper, islet transplantation patients receive whole-body immunosuppression drugs. These drugs can cause various complications and there is a high risk of infection. Considering the risks, Pepper and his team are concerned with answering one question.
“How can we make this procedure safer by reducing the risk and eliminating the need for whole-body immunosuppression or anti-rejection drugs?”
The drug-delivering grafts, developed by Kuppan, involve using microparticles to deliver anti-rejection drugs to newly transplanted islet cells.
“They’re microparticles that we can mix with the cells that we’re transplanting. The cells that need protection are protected by the drugs. They’re just localized, so the whole body isn’t [affected],” Pepper said.
According to Pepper, an islet transplantation is the safest transplant for individuals with T1D.
“We’re hopeful that by delivering the immunosuppressive drugs just to the cells that need them, we can reduce those [complications] and make the procedure safer.”
Research builds on “legacy of the Edmonton Protocol,” Pepper says.
In 2000, a U of A research team developed the Edmonton Protocol. The team included Dr. James Shapiro and Ray Rajotte, both professors in the department of surgery. The Edmonton Protocol is the world’s largest islet transplant program. It has helped at least 255 individuals with T1D achieve insulin independence.
It was the success of the Edmonton Protocol that drew Pepper to the U of A. Here, he completed his postdoctoral studies in the laboratory of Dr. Shapiro.
“What we’re trying to do is build on the legacy of the Edmonton Protocol and continue to refine [the procedure] to make it safer for patients. And by safer, I mean reduce the reliance on whole-body immunosuppression. By doing that, we can make it more inclusive,” Pepper said. “We can protect the cells longer and better so that insulin independence lasts beyond one year and maybe beyond ten years.”
Pepper thinks that by localizing the anti-rejection medicine to just the beta cells, more people will be able to receive the islet transplant.
“Currently we require at least two pancreas donors per recipient to get a person off of insulin, because 70 per cent of those cells die within hours to days,” Pepper said. “We’re hopeful that if we protect those cells, especially post-transplant, then we can just use one pancreas per recipient.”
Currently, Pepper and his team are trying to determine the best anti-rejection drug for protecting transplanted beta-cells. The drugs will be tested on a series of animal models.
“If that looks advantageous, we can leverage the wonderful expertise and infrastructure here at the Clinical Islet Transplant Program and hopefully try this in human patient trials.”




