 Christina Varvis
Christina VarvisThis article is a response to Jon Zilinski’s October 25 editorial, “Mental Health Advocacy is Shit.”
“Shit” is too strong a word to describe mental health advocacy; a more fitting assessment of the movement would be “low-hanging fruit pickers.” Jon has a point: getting people to talk about it can only do so much. Sure, stigma is still a problem — but mental health advocates have a habit of pointing towards a supposed “stigma” without specifying or explaining what in particular is being stigmatized, and what we can do to curb it. Want to be an effective mental health advocate? Stop picking at low-hanging fruit.
“Mental health” is in danger of becoming a buzzword. Mental health advocates need to stop tossing it around in hopes of winning brownie points with the general student populace. Instead, we need to start looking at the myriad of other issues that factor into the complex and multifaceted umbrella-term that is “mental health advocacy.”
There’s a difference between raising “awareness” and raising “education.” Raising awareness can only do so much when misconceptions about mental illness still run rampant. This is how that “grey area” is formed, resulting in many students who know about mental illness but don’t understand it.
Many still think “depression” is synonymous with “sadness.” And that’s technically correct — from a Merriam-Webster standpoint. But if you were to tell me that you’re “depressed” because you don’t have time to binge-watch the new Luke Cage series, I would call you out on your casual insensitivity. There is also a wide array of mental illnesses that don’t get as much attention: developmental disorders (autism, ADHD), personality disorders, as well as the gamut of anxiety-related disorders (excoriation disorder and OCD), to name a few.
As far as stigma goes, one area to zone in on is labeling. Psychiatric labels (and their connotations) are one of the biggest obstacles towards seeking help. Self-labeling is a problem even less people talk about. When someone receives a psychiatric diagnosis, it influences their self-image. At best, it increases self-awareness and motivates positive change; at worst, a diagnosis — or misdiagnosis — leads to a vicious cycle of negative feedback and self-inhibition. This also applies to cases in which people label themselves due to sociocultural influences (like their friends and the media), so more often than not, self-labeling becomes a self-fulfilling prophecy. You are not your diagnosis.
No two individuals with the same diagnosis are going to warrant the same treatment. And yet, we live in a culture that holds the medicalization of mental illness to high regard — a system that inevitably veers towards a one-size-fits-all standard. While psychiatry is a tried-and-true method, there are many who don’t benefit from this approach. In many cases, medication does more harm than good.
Psychiatry, by design, takes a somewhat objective, systematic approach to treating mental illness. This lends itself to non-humanistic tendencies — namely, a tendency to pay more attention to symptoms than the person. This effectively reduces a complex human being to a case study.
The problems inherent in the psychiatric model described above are further exacerbated by the overcrowding of the system with new patients. As a result, it becomes increasingly difficult for physicians to treat patients on a case-by-case basis. Most people require specialized action plans tailor-made to fit their needs.
Many of the action plans given by psychiatrists can be summarized as follows: “Take these meds for a month, see how you feel, then get back to me. If that doesn’t work, we’ll try another one.”
Say what you want about the pharmaceutical industry, but something about implementing trial-and-error methodology seems off to me. Throw in the fact that these medications have the potential to fundamentally alter your brain chemistry — possibly in adverse and unpredictable ways — then your treatment plan is comparable to playing roulette with your brain chemistry.
University students especially can’t afford to experiment with their brain chemistry — not when faced with everything that’s demanded of them on a daily basis.
If the mainstream consensus is that the pharmaceutical route is the first and only resort to mental health treatment — downplaying the benefits of simple lifestyle changes that involve diet, exercise, etc. — then something is terribly wrong.
The medical route needs to be knocked off its pedestal — and mental health advocates need to further promote the alternatives. What has worked for me, for example, has been implementing major lifestyle changes. I’ve also greatly benefited from counselling, and, more recently, from changing my diet under the guidance of a naturopath.
Diet remains one of the most overlooked aspects of supporting one’s mental health. (Shout-out to probiotics.) Others tout the benefits of cognitive behavioural therapy (CBT) and mindfulness meditation. These practices put the agency back in the hands of the individual — and need to be advocated for more strongly and more often.
Ultimately, any advice or treatment you get from any expert should be regarded as guidance more than anything. Our health-care professionals are human beings too, prone to error just like everyone else. When it comes to your mental health, you are the expert on yourself.
Mental health advocacy in general has been successful in raising awareness and encouraging people to seek help (which is still important), but it needs to broaden its focus towards other important aspects of this complex and wide-ranging issue. Stop picking at low-hanging fruit: you’re not saying anything we haven’t heard a million times before.
Actions speak louder than buzzwords.





It is interesting to see someone
critiquing the vagueness of the term “stigma”, while also using the layman term
“brain chemistry”, trivializing the education and knowledge of
psychiatrists as well as pharmaceutical experts, and, finally, “shouting
out to probiotics”.
It takes an incredible amount of cognitive dissonance and misguided hubris to
criticize advocates for picking at “low-hanging fruit” and pointing out that professionals
find it difficult to individualize treatment while, simultaneously, recommending the promotion of incredibly vague
“lifestyle changes” prescribed by a naturopath (not by a dietician,
for some reason) because it worked for you.
Here, let me sum up this article in the same way it attempts to downplay the rigorous
training of medical professionals: “People need specialized treatment, but
naturopathy worked for me. Those rigorously screened, highly knowledgeable
doctors might disrupt your brain chemistry , and that’s
bad (citation, another article by a fellow Gateway writer)
Shout-out to probiotics!”
Actions speak louder indeed, but all this article offers is buzzwords and
grocery recommendations.
What kind of neurotypical, ableist BS is this article. “Change your diet!! Go outside more!! That’ll cure your mental health! Definitely not drugs!”
Did the article say this? The author’s simply saying that, because the current mental health framework is so obviously flawed, those facing mental health problems may find solutions from alternative sources.
But the author never starts to consider that implementing solutions for the flaws within the current mental health framework would be much more effective than going to some of these alternatives. Of course everything engaged with mental illness treatment is consistently trying to improve it – it’s not just about prescribing drugs and seeing what happens. But you shouldn’t be able to rule that out completely like the author does.
It’s a Gateway article, not an honors thesis. There’s only so many directions one can go with a 900-word limit. Besides, this author isn’t a doctor — it shouldn’t be his job to propose changes to the complexities of the healthcare system. If he did, he’d likely be criticized for acting like an expert on a topic he isn’t qualified to speak about.
All these pissed off pre-med students seem to be missing the point of the article. Get off your high horse and take the criticisms mental health patients have seriously.
Dear anonymous commenter,
If you have a problem with me, which you clearly do, feel free to email me at [email protected] so we can meet up in person. I’d very much like to talk to you — because I know it’s only you commenting these things, from a time zone two hours ahead of Edmonton’s — and meet the sad little person who feels compelled to call me a bitch and a whore and a loser anonymously on Gateway articles.
Sincerely,
Kate McInnes
You really woke up at 4:30 am to write this comment? If you’re on the Gateway this early, try reading the articles and making comments that grapple with the topics and opinions brought up by their writers instead of worrying about me. Thanks for the attention though 🙂
This starts out alright, and then it veers into some of the most uneducated, inaccurate, meaningless drivel I’ve ever read about mental health. As a mental health professional, I am genuinely ashamed that my alma mater would print this.
“Psychiatric labels (and their connotations) are one of the biggest obstacles towards seeking help.”
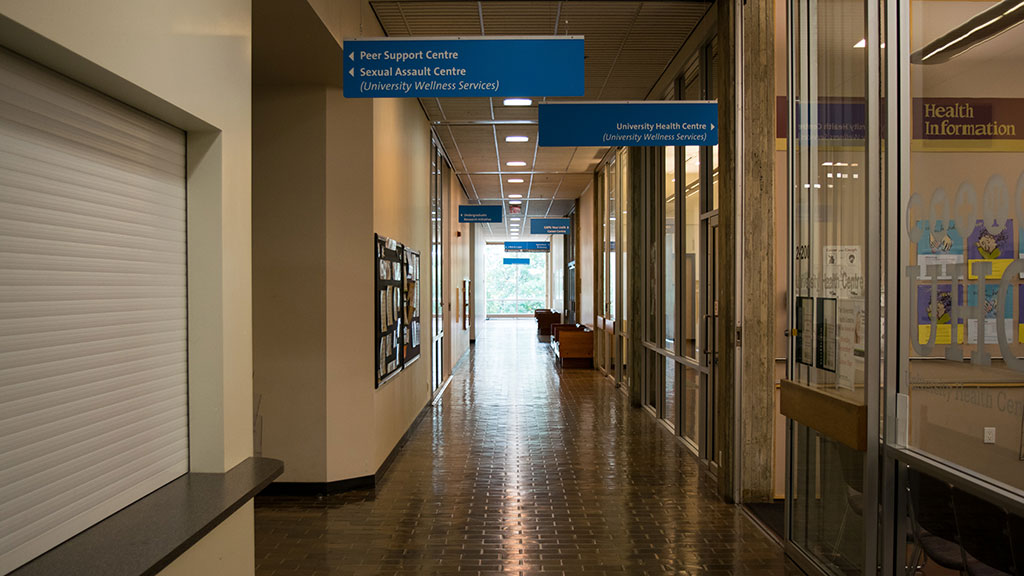
Are they? Because when I worked in the university’s mental health system, students who came to see the school-employed psychologists or psychiatrists were often placed on 8-week long waiting lists – or longer – unless they were in immediate crisis. You want to find fault with the university’s mental health services? I’d start there.
“Many of the action plans given by psychiatrists can be summarized as follows: “Take these meds for a month, see how you feel, then get back to me. If that doesn’t work, we’ll try another one.””
And do you know why that is? As you were gleefully condemning the entire field of psychiatry, did you ever stop to think that there might be a good reason for this? People respond to psychoactive medications differently. While Sally might feel like her old self on Wellbutrin, maybe Peter feels better on Prozac. And, surprise surprise, it takes a full month of taking antidepressants before they start to kick in. Psychiatrists are not saying “take this for a month and get back to me” because they’re pill-dispensing robots; that is genuinely the best course of action for you to take, in addition to whatever talk therapies and lifestyle changes you can manage.
“Say what you want about the pharmaceutical industry, but something about implementing trial-and-error methodology seems off to me. Throw in the fact that these medications have the potential to fundamentally alter your brain chemistry — possibly in adverse and unpredictable ways — then your treatment plan is comparable to playing roulette with your brain chemistry.”
You know why it seems off to you? Because you have no idea what you’re talking about. Something about injecting yourself with pancreatic secretions every day to alter your blood chemistry seems “off” to me, but it seems to work for diabetics. If you have a chemical imbalance in your brain that’s making your life miserable – like, say, with bipolar disorder, or treatment-resistant depression – altering your brain chemistry is the entire point. And despite what you seem to believe, psychiatrists are not handing you mystery pills out of a bowl just to see what happens. The side effects of psychoactive medication are not “unpredictable” – they are clearly listed on drug information sheets, along with their likelihood, and your doctor or pharmacist would be happy to discuss anything that you might be concerned about.
“If the mainstream consensus is that the pharmaceutical route is the first and only resort to mental health treatment — downplaying the benefits of simple lifestyle changes that involve diet, exercise, etc. — then something is terribly wrong.”
But nobody is saying that. Mental health professionals aren’t saying that. The very editorial you’re poo-pooing was complaining about mental health advocacy and its focus on healthy lifestyle. But if you genuinely think that bipolar disorder, or anorexia nervosa, or schizophrenia, or borderline personality disorder, or persistent depressive disorder can be cured by a brisk jog and a tub of probiotic yogurt, without the assistance of a mental health professional, then I invite you to step away from the keyboard because you are genuinely a menace to student health and safety.
“The medical route needs to be knocked off its pedestal — and mental health advocates need to further promote the alternatives. What has worked for me, for example, has been implementing major lifestyle changes. I’ve also greatly benefited from counselling, and, more recently, from changing my diet under the guidance of a naturopath.”
And that’s great that it worked for you. Really. But it’s rich to see an article that disparages medication as ineffective heap praise upon a naturopath. Psychoactive medication has been studied and proven to have an effect. Naturopaths have been studied and proven to be nothing but an expensive placebo. If you feel better under the guidance of a naturopath, that’s wonderful for you, but they are not knowledgeable about mental illness, and their advice on how to handle a developmental disorder, or treatment-resistant depression, or a brain chemistry disorder like Bipolar disorder is completely and categorically useless. Sending someone with a serious mental health issue to a naturopath as a first plan of action is just delaying them from getting real help.
“Ultimately, any advice or treatment you get from any expert should be regarded as guidance more than anything. Our health-care professionals are human beings too, prone to error just like everyone else. When it comes to your mental health, you are the expert on yourself.”
And if your doctor tells you that your blood sugars are too high, should that be regarded as guidance? Or if he tells you your thyroid isn’t functioning properly, should that be considered mere “guidance”? After all, you are the expert on yourself.
People in their late teens and early twenties, particularly those under a great deal of constant stress are at some of their highest lifetime risk for developing a serious mental health issue, above and beyond a simple case of the blues. Many students, during their time at university, will develop serious, debilitating depression or anxiety, eating disorders, bipolar disorder, schizophrenia, and so many more. They will need professional help – I don’t have to remind anyone that the school endures the tragic loss of its own students to suicide every single year. If the university is serious about stepping up its efforts to help students with mental illness, they need to dramatically step up the number of clinical psychologists and psychiatrists available to see students, dramatically increase translation services or non-English mental health services for international students, educate all educational staff and advisors on how to identify students that might be struggling, and make it easier for students to take time off school for mental health reasons without financial or academic consequences.
They don’t need to keep printing garbage like this.
For someone who claims to work in the field of mental health, this comment is needlessly mean-spirited. You clearly took offence at his critique of your questionable profession. The author makes some very valid arguments based on his own experiences, and to say that he has “no idea what [he’s] talking about” undermines that experience. I admire this author for making such controversial points, and your comment supports his argument that mental health professionals don’t understand — or care to understand — the variety of problems that exist within the current failing mental health framework.
—-Sure, stigma is still a problem
I think you entirely miss the point, people who say there is a stigma are the problem. People who declare their prejudice, their acts of discrimination are justified by saying it is someone else’s
stigma.
It is what you have been taught to say. You will have to teach yourself to stop, if you can.
It will take personal resolve, but you can
Harold A. Maio, retired mental health editor [email protected]