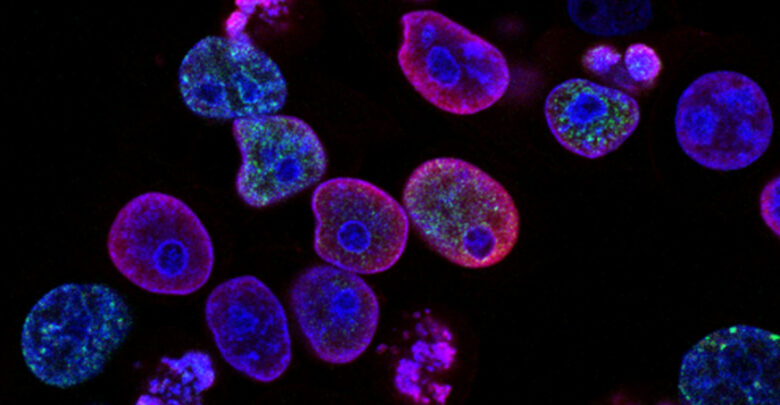
 National Cancer Institute
National Cancer InstituteKhaled Barakat, a University of Alberta professor in the faculty of pharmacy and pharmaceutical sciences, has recently identified a potential small molecule drug that could make use of the body’s own immune system to combat cancer.
T-cells are white blood cells and a part of the immune system. They play an important role in the body’s natural defense against cancer and other pathogens, Barakat said. In patients with cancer, their T-cells can become less active in a phenomenon known as T-cell exhaustion.
“Think about T-cells as like the police officers in the immune system,” Barakat said. “Our idea is to develop small molecule drugs that can reactivate these T-cells.”
This idea of harnessing the immune system to kill cancer cells is not new. Antibody therapy, which involves injecting antibodies to stimulate immune cell activation, works by roughly the same principle. Small molecules hold an advantage over other larger immune-activating molecules like antibodies in that their dosing can be controlled more finely, according to Barakat.
Antibodies are typically given via injection once every couple of weeks, Barakat said. Once injected, it can be difficult to stop the antibodies from working. This can potentially result in them over-activating the immune system, according to Barakat.
In the worst case, patients can experience “huge side effects, like severe rash and diarrhea.” Small molecules on the other hand are taken orally every few hours. “If you get the side effect, you can just stop the treatment,” Barakat said.
Barakat’s lab uses generative AI to model molecules
To find and develop these potential small molecule drugs, Barakat’s lab focuses on the use of generative artificial intelligence (AI). When looking for potential drugs manually, researchers run the risk of missing the bigger picture, Barakat said.
“It is like an ant that is working on a single leaf and ignoring that there are many leaves on other trees,” Barakat said. With AI, the lab can create custom molecules that have maximum cancer-fighting effectiveness and minimal unwanted side effects.
Now that the researchers have confirmed the drug’s activity in cells, the next step is to demonstrate non-toxicity and effectiveness in animal cancer models, Barakat said. There, the researchers will work out the specifics of how to administer the drug in humans.
Eventually, with success in animal studies, the hope is for the drug to enter clinical trials. After five years of work, the compound has hit the midway point in the drug development process.
“It’s a very difficult process,” Barakat said. “All this excitement that we have right now could [be in] vain” if the drug fails to show benefit in animal models.
Barakat stressed that this research is not the work of their lab only. “It is a multi-disciplinary drug discovery [process],” one that Barakat said wouldn’t be possible without a team of collaborators all across the U of A.
”It is transformative to have this kind of a salvaging methodology that we’re trying to develop,” Barakat says
While the small molecule drug work continues, Barakat’s lab is simultaneously researching methods to salvage drugs that have been taken off the market due to unacceptable side effects.
“Imagine you develop a drug. You spend billions of dollars on this drug. And suddenly [it has] been discovered that [it] can actually lead to sudden death due to cardiotoxicity,” Barakat said.
To salvage these drugs, Barakat’s lab is using AI to change the molecular structures of these drugs in such a way to prevent unwanted side effects while maintaining the drug’s therapeutic potential.
“It is transformative to have this kind of a salvaging methodology that we’re trying to develop.”




