 Supplied
SuppliedA new COVID-19 tracking bracelet being developed by a team at the University of Alberta hopes to enable physicians to make faster decisions about the medical care necessary for patients.
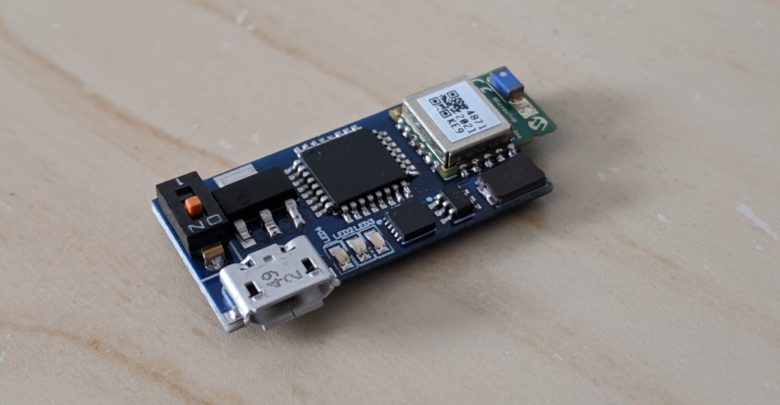
Mitalics Accelerate and iMD Research have joined forces with students and professors from the U of A and McGill University to develop a tracking device which hopes to fill the void left by over-the-phone checkups. Using Bluetooth technology, the bracelet measures four vital signs simultaneously: oxygen saturation, respiratory rate, heart rate, as well as temperature. The signals are converted into vital signs on your mobile phone and the data will then be uploaded to the cloud in real-time, alerting healthcare professionals of cases where immediate action is needed to be taken.
Irene Cheng, a U of A computer science professor working on the project, says the bracelet was originally designed to detect sleeping disorders. However, after the outbreak of the global pandemic, the team’s focus quickly shifted to tackling COVID-19, first by concentrating on already confirmed positive cases before veering course once more, now emphasizing more preventative measures.
“Initially, the main purpose was as a tool for physicians to use to monitor patients who already tested positive for the coronavirus when they had to stay home and isolate,” Cheng said. “The doctors could have the information on hand when they called to check up on their patients.”
“Now, the purpose is to have the device automatically upload the data to the cloud, and from there, an analysis can be done of the vital measures that were recorded.”
According to Cheng, the efficacy of the device depends on recognizing a pattern between the four vital signs that is unique to COVID-19.
“What is important here is that we look at the composite signal, instead of just one individual measure,” she said. “By taking a combination the vital signs, an additional signal pattern is provided.”
Jianfei Ma, a U of A masters of multimedia science student, is contributing to pattern analysis within the project. In terms of differentiating vital patterns, Ma suggests the proper scope in pursuit of analyzing the nature of COVID-19 shouldn’t be short-sighted.
“Vital signs for COVID-19 may be similar to the common cold with your temperature being higher or maybe your heart rate being up” Ma started. “But, if the longer-term patterns show us that over time that heart rate or respiration rate is rising, or one’s temperature is decreasing, it is here where we can classify the pattern as being different than the common cold.”
Naimur Rahman, a U of A computing science student is working on the technological parts of the tracking bracelet, including connecting it to a mobile phone. According to Rahman, mobile phones were ideal for receiving the data from the device because they have the right amount of processing power.
“We selected Bluetooth to connect the device to a mobile phone, which will not use an excessive amount of energy to get the signals recorded by the device,” Rahman stated “Once the data is received by the mobile phone, we will run the algorithm we have developed to convert it into the vital signs for each of the four vitals being measured.”
Once the artificial intelligence (AI) of the tracking bracelet is done, Rahman’s next step is improving the accessibility of the vitals for patients.
“Once we develop the AI system we are currently working on, we can also try to place [the AI] in the mobile phone so the user of the device can also have information at their fingertips about the patterns and composite patterns they’re displaying.”
The device also has another main function: tracking. Although an abundance of contact tracing software is available in the market at the moment, Cheng suggests what the device she and her team are working on is beyond what is currently available.
“Other than checking to see if a person is positive and contacting everyone they have been around, we also want to add some statistics,” she said. “For example, knowing more about an area that has a lot of positive cases and putting this information on google maps. Is this area more multicultural? Are there more restaurants in this particular area?”
One hurdle the team has faced is the bracelet currently relying on the users mobile phone to determine the location of the user. This is a concern for particular demographics of people in society, such as senior citizens, who do not typically have cell phones.
Despite this minor obstacle, Cheng asserts that the software on its own will be more or less available by the end of the year.
The team remains confident in the device’s potential to make an impact, whether it’s scoping out the coronavirus or other health conditions
“We’ve been doing signal processing for a long time, not just for COVID-19,” Cheng said. “Any personal health data will show a pattern.”